Dec 31, 2025
Voice AI for Patient Registration in Healthcare
Patient registration is one of the most critical yet overlooked workflows in healthcare operations. Manual processes, long hold times, and overloaded front desks not only frustrate patients but also inflate administrative costs that already burden providers globally.
In fact, the global AI voice agents market in healthcare is projected to grow from $468 million in 2024 to $3.18 billion by 2030, driven by demand for automation that cuts costs and improves efficiency. For hospitals and clinics dealing with high call volumes, legacy IVRs and repeat callbacks are more than inconveniences; they translate to lost revenue, lower patient satisfaction, and delayed clinical care.
This blog cuts through the noise to show you why voice AI is reshaping patient registration, how it affects key healthcare KPIs, and what capabilities your enterprise must evaluate to succeed.
Key Takeaways
Patient registration voice AI directly impacts cost, compliance, and patient experience at scale.
Voice AI enables faster, more accurate, and always-on registration without adding staff.
Indian healthcare benefits strongly due to language diversity and high call volumes.
Success depends on healthcare-ready workflows, compliance, and human escalation.
CubeRoot enables scalable, compliant patient registration voice AI with rapid deployment.
Why Patient Registration Has Become a Cost and Experience Risk for Healthcare Providers?
Patient registration has quietly shifted from a back-office task to a frontline risk area for your operations and patient experience. As patient volumes rise and expectations mirror consumer-grade service, every delay or error at registration compounds into financial loss, compliance exposure, and trust erosion.
Here are the core reasons patient registration voice AI now puts both cost and experience at risk for you:
Revenue Leakage From Incomplete Registrations: When insurance details, IDs, or consent are missed or partially captured, claims get delayed or denied, directly impacting your cash flow.
Higher No-Show Rates From Poor Pre-Visit Engagement: If patients are not registered or appropriately reminded, appointments drop off, leaving your doctors underutilized.
Compliance Exposure at Scale: Manual scripts and ad-hoc calls increase the risk of consent gaps and audit failures as volumes grow.
Operational Fragility During Demand Spikes: Seasonal surges, outbreaks, or camp registrations strain fixed teams and break consistency across locations.
As these cost and experience pressures intensify, healthcare providers are increasingly looking toward voice AI to fundamentally redesign how patient registration voice AI actually works.
What Does Voice AI Change in the Patient Registration Workflow?
Voice AI fundamentally reshapes how registration happens by removing friction from the earliest point of patient interaction. Instead of forcing patients to adapt to rigid systems or wait for staff availability, you let registration adapt to patient behavior, timing, and language.
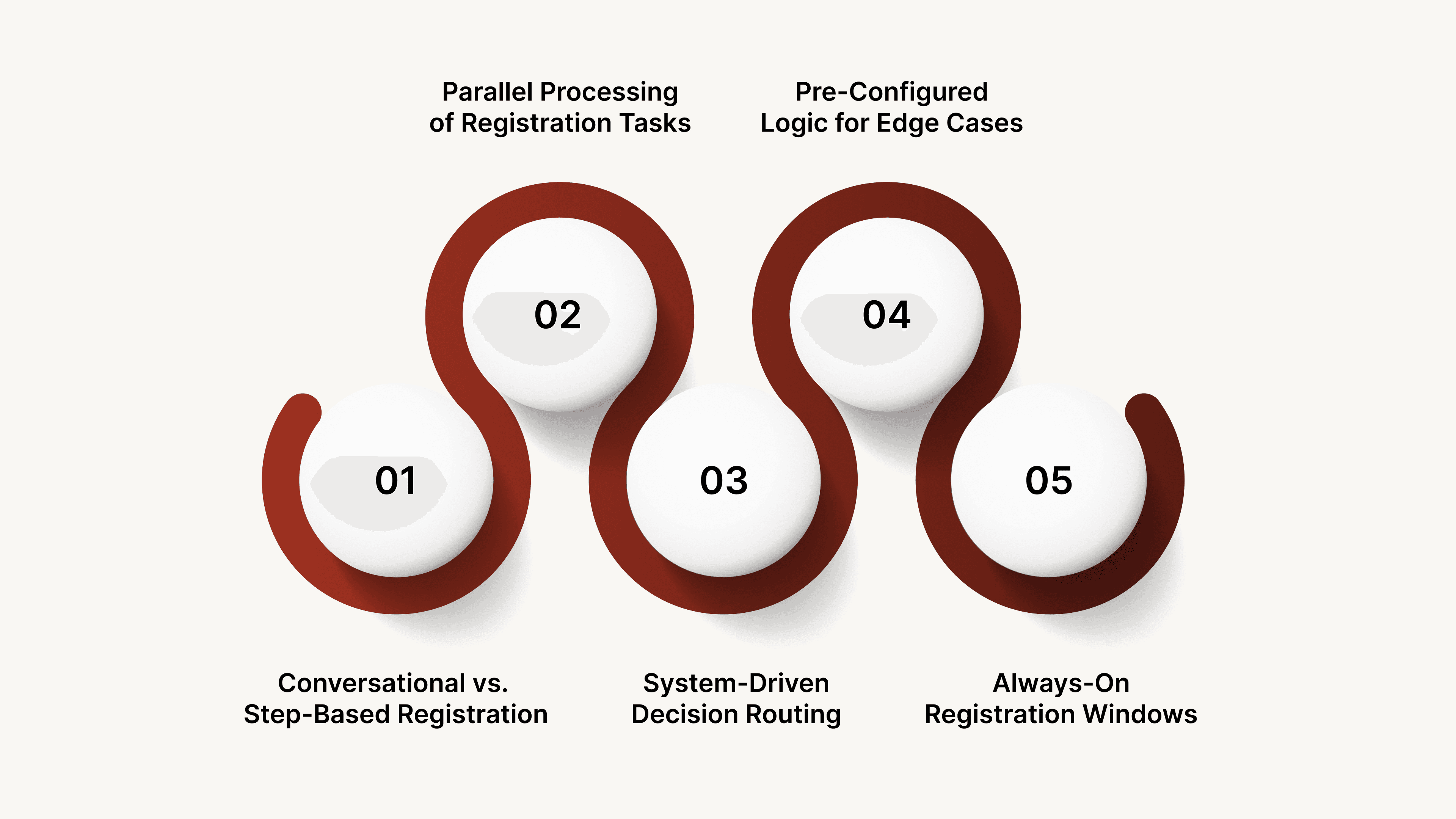
Below are the key workflow-level changes you unlock with Voice AI:
Conversation-Led Registration Instead of Step-Based Calls: You guide patients through registration naturally, allowing interruptions, clarifications, and corrections without restarting the process.
Parallel Processing of Registration Tasks: You collect demographics, visit intent, and eligibility details within a single interaction instead of splitting them across multiple calls.
Pre-Configured Logic for Edge Cases: You handle scenarios like first-time visitors, follow-up consults, or referral-based visits without manual intervention.
Always-On Registration Windows: You allow patients to complete registration outside clinic hours, reducing next-day congestion and walk-in pressure.
Also Read: Everything You Need to Know About AI Assistants
Once the workflow-level impact of voice AI is clear, the next step is identifying where it delivers the greatest operational value within real patient registration voice AI scenarios.
Top 5 High-Impact Patient Registration Use Cases for Voice AI
Patient registration is not a single interaction. It spans multiple touchpoints before, during, and sometimes after a visit. Voice AI becomes most valuable when it is applied selectively to high-friction moments that repeatedly consume staff time or delay patient movement.
For healthcare enterprises managing multiple specialties, locations, or digital channels, identifying these moments is what drives measurable impact.
Below are the most impactful patient registration scenarios where Voice AI fits naturally into your workflow.
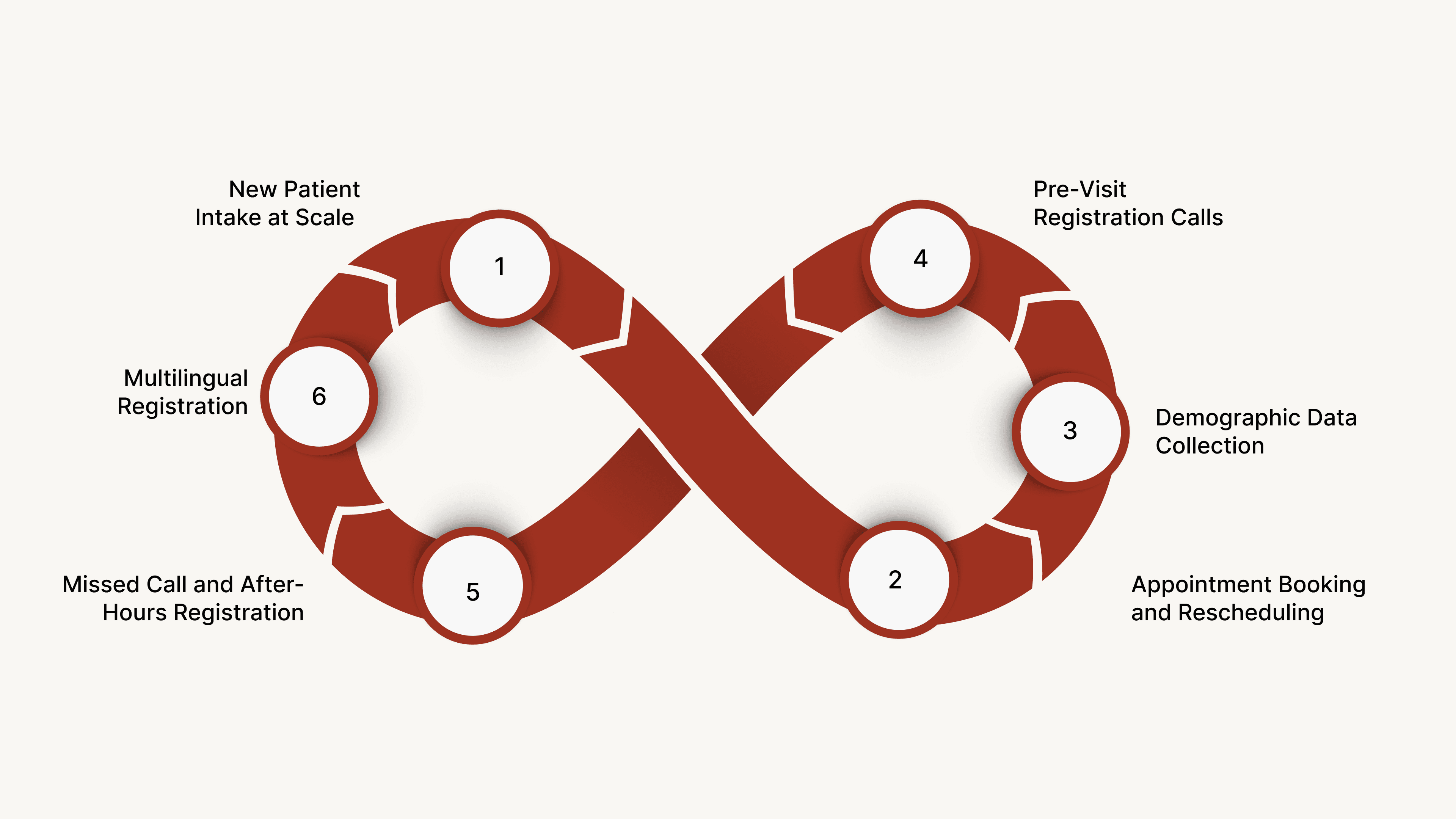
New Patient Intake at Scale
New patient intake is where the scale breaks most healthcare systems. Marketing campaigns, physician onboarding, insurance empanelments, or seasonal demand can suddenly push thousands of first-time callers into your ecosystem.
Below are the core ways Voice AI strengthens new patient intake at scale:
Structured First-Contact Data Collection: Patient details are captured in a standardized format from the first call, reducing downstream clarification cycles.
Specialty and Visit-Type Identification: Callers are guided to the correct department or doctor based on symptoms or visit purpose.
Faster Onboarding for New Clinics or Doctors: Intake workflows adjust quickly when new providers or services are added.
Reduced Abandonment During High Traffic: Callers complete the intake without waiting for availability during peak demand.
Appointment Booking and Rescheduling
Appointment booking and rescheduling directly shape how efficiently clinical capacity is utilized. Missed calls, delayed callbacks, and limited booking windows quietly waste available slots every day.
Below are the key ways Voice AI transforms appointment booking and rescheduling:
Real-Time Slot Discovery and Confirmation: Available slots are checked and locked instantly during the call.
Automatic Rescheduling for Cancellations: Open slots are refilled quickly by routing eligible patients without staff involvement.
Visit-Type Based Scheduling Logic: Consults, follow-ups, diagnostics, and procedures are scheduled with the correct duration.
Reduced Back-and-Forth Communication: Patients finalize bookings in one interaction instead of multiple follow-ups.
Insurance and Demographic Data Collection
Insurance and demographic data collection is where small inaccuracies create oversized operational friction. Policy numbers, payer names, address details, and identity fields often arrive incomplete or inconsistent, forcing multiple verification touchpoints later. Below are the key ways Voice AI strengthens insurance and demographic data collection:
Guided Field-by-Field Data Capture: Information is collected in a controlled sequence, reducing skipped or misaligned entries.
Real-Time Data Confirmation With Patients: Critical details are repeated back and corrected during the same interaction.
Support for Multiple Payers and Plans: Insurance logic adapts across private insurers, government schemes, and corporate coverage.
Reduced Dependency on Follow-Up Calls: Complete profiles minimize the need for staff-led verification later.
Pre-Visit Registration Calls
Pre-visit registration calls determine how smoothly a patient moves from scheduling to consultation day. When these calls are missed or rushed, patients arrive unprepared, causing delays, rescheduling, or longer wait times.
Below are the ways Voice AI strengthens pre-visit registration workflows:
Advance Collection of Mandatory Details: Forms, IDs, and visit prerequisites are confirmed before the appointment date.
Procedure-Specific Preparation Guidance: Patients receive clear instructions based on the nature of the visit or test.
Automated Outreach at the Right Time: Calls are triggered based on appointment proximity instead of manual scheduling.
Reduced Day-Of Registration Congestion: Front desks handle fewer incomplete check-ins.
Also Read: Customer Service vs Customer Support- Key Differences Explained
Missed Call and After-Hours Registration
Missed calls and after-hours inquiries represent a silent demand that most healthcare systems fail to convert. Patients often call during evenings, early mornings, or short breaks, and a single unanswered attempt can push them to another provider.
Below are the key ways Voice AI strengthens missed call and after-hours registration:
Instant Call-Back Registration Flows: Missed calls automatically trigger a return interaction that captures patient intent and basic details. This prevents loss of high-intent callers who are unlikely to call repeatedly.
After-Hours Appointment Intent Capture: Patients register visit requirements even when clinics are closed. These inputs are queued for scheduling without waiting for office hours.
Reduced Dependence on Manual Follow-Ups: Registration data is already structured when staff review it later. This shortens response time and avoids repeated clarification calls.
Consistent Experience Across Time Windows: Patients receive the same guidance at night as during business hours. This consistency builds trust and improves perceived accessibility.
Losing patient inquiries because calls go unanswered after hours or during peak load? CubeRoot’s missed-call and after-hours Voice AI automatically calls patients back, captures registration details, and queues visit intent. Never lose high-intent patients due to timing or call volume again.
After understanding where voice AI creates the most impact within registration workflows, its effectiveness in Indian healthcare must be matched by strict compliance and governance standards.
What Compliance and Governance Standards Must Be Met?
Patient registration through Voice AI touches regulated data at the very first interaction. Identity details, medical context, and consent are collected before any clinical engagement begins. Without strong governance, automation can amplify risk instead of reducing it.
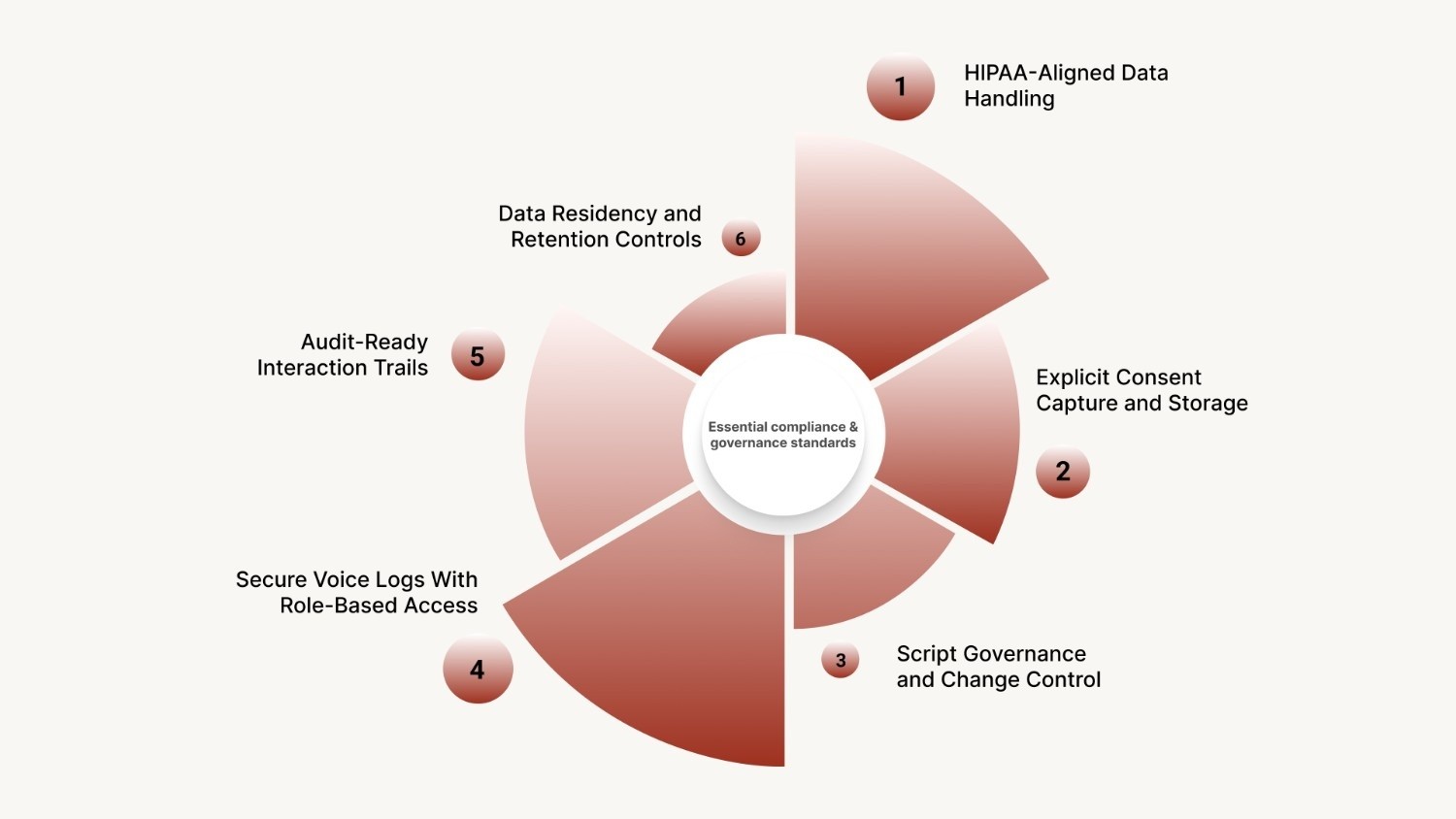
Below are the essential compliance and governance standards that must be embedded into your Voice AI registration workflows:
HIPAA-Aligned Data Handling: Patient information is captured, stored, and transmitted using encryption and access controls aligned with global healthcare data protection standards.
Explicit Consent Capture and Storage: Verbal consent is recorded, timestamped, and linked to each registration record. This creates defensible proof during audits or dispute resolution.
Script Governance and Change Control: Registration prompts follow approved language that cannot be altered without authorization. This prevents accidental deviations across teams or locations.
Secure Voice Logs With Role-Based Access: Call recordings are retained securely and accessed only by permitted roles. This limits exposure while preserving traceability.
Audit-Ready Interaction Trails: Every step in the registration flow is logged for review. Compliance teams can trace who was contacted, what was said, and how data was captured.
Also Read: Interactive Voice Response (IVR) Meaning Explained
Even with strong compliance frameworks in place, voice AI initiatives can still fall short if common implementation and adoption pitfalls are not addressed early.
What Are the Common Failure Points in Voice AI Adoption for Healthcare?
Voice AI adoption in healthcare often fails not because of the technology, but because of how it is implemented and governed. When systems are deployed without clinical context, operational alignment, or escalation safeguards, they create frustration instead of efficiency.
Below are the most common Voice AI adoption risks in healthcare, along with practical solutions.
Failure Point | Practical Solution |
|---|---|
Generic conversation design | Use healthcare-trained workflows aligned with clinical context |
Limited language and accent support | Deploy India-trained, multilingual speech models |
No escalation for sensitive cases | Enable human-in-the-loop escalation |
Disconnected backend systems | Integrate scheduling, billing, and patient systems via APIs |
Over-automation without oversight | Add monitoring dashboards and review loops |
Rushed go-live timelines | Roll out in phases with validation before scale |
Understanding where voice AI deployments commonly fail helps healthcare enterprises evaluate vendors more critically and avoid repeating the same mistakes.
How Should Healthcare Enterprises Evaluate Voice AI Vendors?
Selecting a Voice AI vendor for patient registration is a long-term operational decision, not a pilot experiment. The system becomes part of how patients enter your care ecosystem, which means early trade-offs compound quickly.
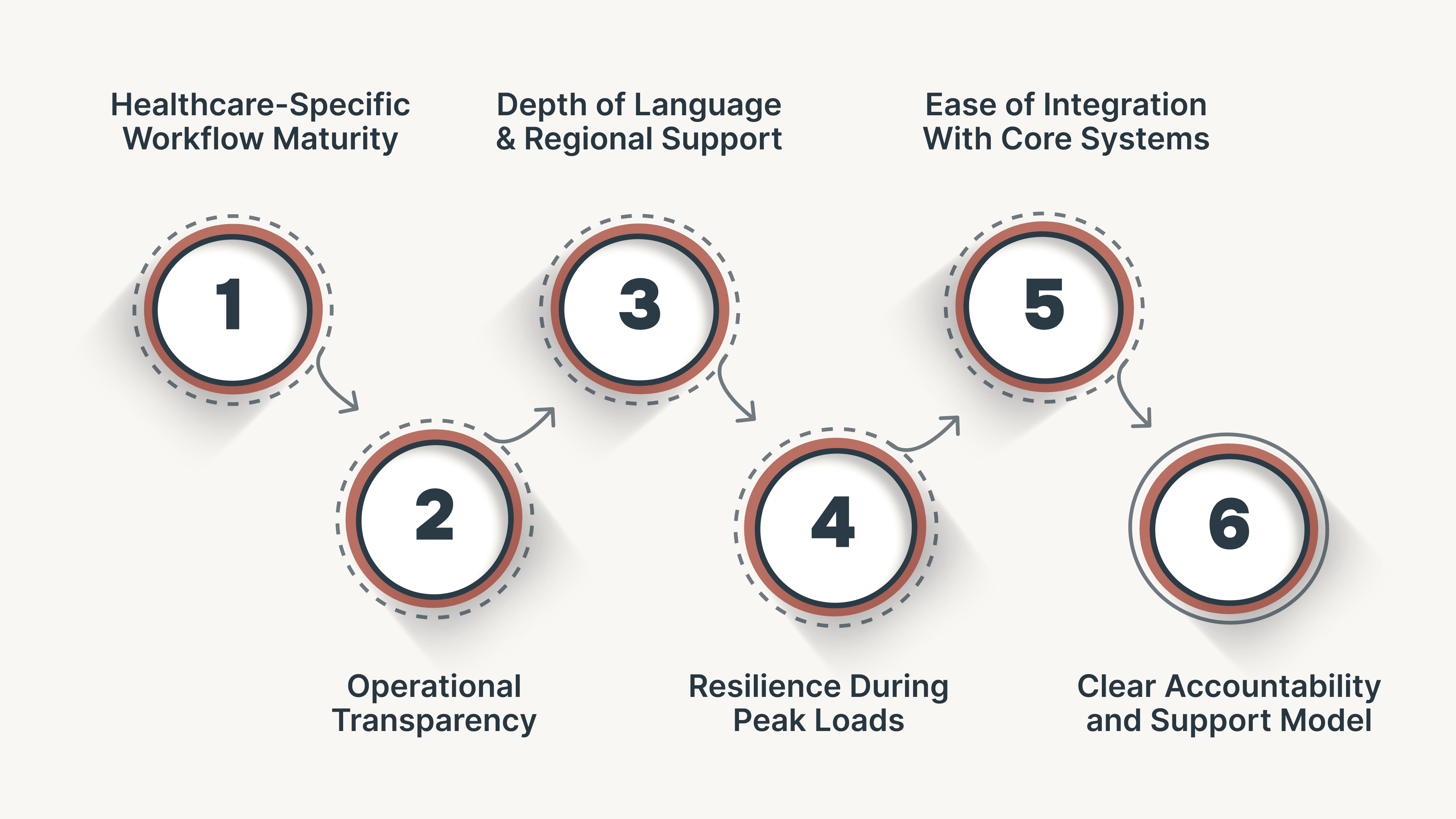
Key evaluation criteria:
Healthcare-Ready Workflows: Registration flows should already support visit types, payer logic, and patient categories without heavy customization.
Operational Visibility and Control: Dashboards must provide insight into call flows, outcomes, and exceptions, with the ability to make quick changes in-house.
Language and Regional Coverage: Voice AI must handle mixed-language conversations and regional accents common across India.
Scalability Under Load: Performance should remain stable during peaks from camps, outbreaks, or high-volume drives.
Clear Ownership and Support: Accountability for uptime, compliance, and performance must be well-defined beyond initial deployment.
Also Read: How AI is Transforming Call Centres and Customer Service
Once evaluation criteria are clear, the next step is seeing how a healthcare-focused platform like CubeRoot meets these requirements in practical patient registration environments.
How CubeRoot Powers Scalable, Compliant Patient Registration
Patient registration voice AI at enterprise scale requires more than automation. CubeRoot is built to meet these exact requirements in Indian healthcare environments, where registration workflows must balance speed, compliance, and patient trust simultaneously.
Below is how CubeRoot enables scalable and compliant patient registration in practice:
Prebuilt Healthcare Workflows: Ready registration flows cover first visits, follow-ups, diagnostics, and specialty routing, reducing setup time.
Compliance-Ready Conversations: Consent capture, script control, and secure recordings are embedded, keeping interactions audit-ready without added overhead.
Multilingual Voice Agents: Native support for regional languages, accents, and mixed-language conversations ensures consistent patient experiences.
Human-in-the-Loop Escalation: Sensitive or complex cases route to live staff with full context, avoiding repetition and trust gaps.
Fast, Integrated Deployment: No-code tools and APIs connect registration, scheduling, and insurance capture directly with HIS and EHR systems.
For healthcare providers aiming to improve access, reduce administrative strain, and scale patient intake without compromise, CubeRoot delivers a registration layer built for practical complexity.
Conclusion
Patient registration is no longer just an administrative step. It is the first real interaction patients have with your healthcare system, and it shapes trust, efficiency, and downstream outcomes. As volumes increase and expectations evolve, voice-led registration offers a practical path to scale access without increasing operational strain.
CubeRoot enables this shift by combining healthcare-trained voice intelligence with enterprise-grade scalability and governance. CubeRoot supports registration workflows that remain consistent under pressure while improving patient experience across touchpoints.
If improving registration efficiency, reducing manual load, and scaling patient access are priorities, the next step is simple. Book a demo with CubeRoot to see how voice-led patient registration can fit into your healthcare operations.
FAQs
1. Can Voice AI handle emergency or urgent healthcare calls during registration?
Voice AI is not designed to replace emergency response systems, but it can identify urgent signals during registration calls. When keywords indicating distress or emergencies are detected, the system can immediately escalate the call to live staff or redirect patients to appropriate emergency services.
2. How does Voice AI manage patient identity verification without physical documents?
Voice AI verifies identity using structured verbal confirmation, such as full name, date of birth, phone number, and government ID references. These inputs are cross-checked against backend systems.
3. What happens if a patient provides conflicting or unclear information during a call?
Voice AI can pause the flow, ask clarification questions, and reconfirm critical fields in real time. If inconsistencies persist, the interaction is flagged and routed for manual review, ensuring inaccurate data does not enter clinical or billing systems.
4. Can Voice AI support registration for diagnostics, labs, and imaging centers?
Yes, Voice AI can manage registration for labs and diagnostic centers by capturing test type, referring doctor details, preferred time slots, and patient demographics. This is especially useful for high-volume centers where walk-ins and phone bookings need structured intake.
5. How is Voice AI performance monitored and improved over time in healthcare use cases?
Performance is tracked through metrics like completion rates, error flags, call duration, and escalation frequency. These insights are reviewed regularly, and conversation flows are refined using real interaction data.























