Dec 26, 2025
AI Voice Agents in Healthcare Workflows
India’s healthcare ecosystem is evolving rapidly, yet communication workflows remain under pressure as patient volumes rise. You manage growing appointment requests, chronic care follow-ups, test-result updates, and discharge check-ins across multiple departments.
Non-communicable diseases (NCDs) are now estimated to account for 63 percent of all deaths in India, according to recent UNDP data. With this rising burden, relying entirely on manual calling teams to manage patient interactions is no longer scalable. AI voice agents enable you to automate high-volume interactions, ensure consistent patient communication, and free clinical teams for higher-value tasks.
Key Takeaways
AI voice agents improve workflows that rely on timely, structured patient communication.
Departments get cleaner, standardised clinical inputs without increasing manual calling effort.
Speciality teams benefit when question paths and escalation rules match their protocols.
Integrations with HIS or EHR systems keep patient information updated across units.
Piloting in high-volume departments helps validate performance before wider rollout.
Voice automation provides consistent communication even during peak load periods.
Why Healthcare Providers in India Need Voice Automation
Healthcare providers in India manage high call volumes every day. You handle appointment requests, report-status queries, discharge follow-ups, and insurance-related questions across multiple departments. As volumes rise, maintaining consistent patient communication becomes increasingly difficult.
Several challenges drive the need for voice automation:
High patient traffic: Daily peaks across OPD, diagnostics, and emergency care increase the load on response teams.
Staff shortages: Most hospitals operate with limited administrative capacity, which leads to long wait times and dropped calls.
Operational delays: Manual follow-ups for appointments, reminders, and chronic care check-ins consume significant staff hours.
Seasonal demand spikes: Flu seasons, health camps, and corporate checkup cycles create unpredictable call surges.
Voice automation helps you manage these routine interactions at scale. You can automate reminders, follow-ups, symptom check-ins, and basic information queries without adding headcount. You also ensure faster responses and more reliable communication, which improves overall patient experience.
Must read: Interactive Voice Response (IVR) Meaning Explained
What Are AI Voice Agents for Healthcare?
AI voice agents for healthcare are automated conversational systems that handle clinical and administrative tasks with precision and context. They go beyond standard IVR flows and respond intelligently based on patient inputs and predefined medical workflows.
These agents support specialised tasks such as:
Collecting structured symptom information using clinically designed question paths.
Confirming medication adherence through simple, guided interactions.
Verifying patient identity before sharing report-related or appointment-specific details.
Documenting patient responses directly into your HIS, EHR, or CRM systems.
They can also recognise intent, switch languages as needed, and escalate to your team when a case requires human involvement.
You can deploy them for both inbound and outbound interactions, allowing you to manage critical patient workflows with speed, consistency, and minimal manual effort.
Suggested read: Voice Bots in Healthcare: Top 7 Use Cases Every Hospital Should Know
Key Healthcare Workflows Voice Agents Can Transform
AI voice agents have the most significant impact when they handle workflows that require timely, structured, and repetitive patient communication. These workflows follow clear steps, rely on accurate data capture, and often see high call volumes across Indian hospitals and diagnostic networks.
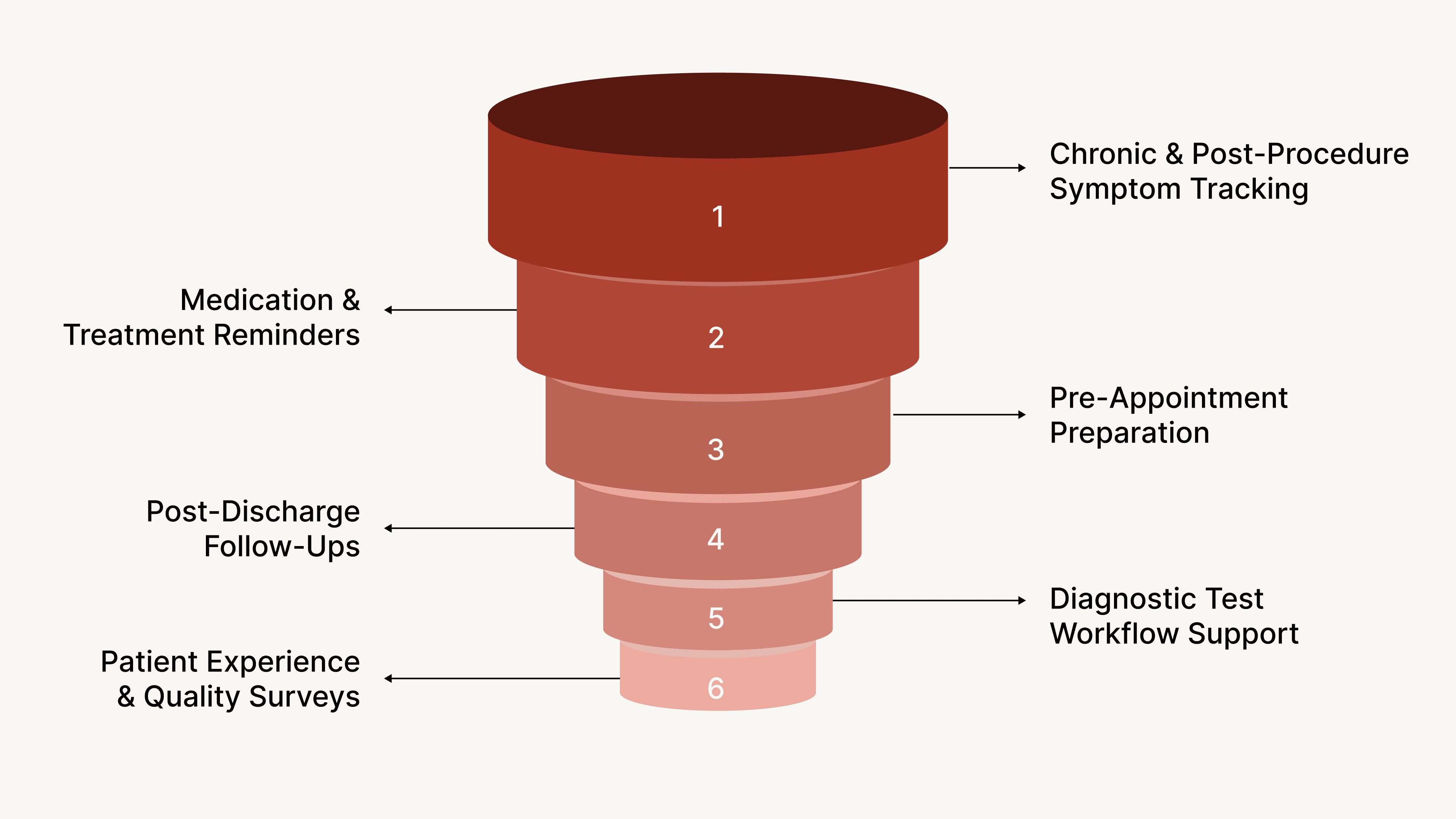
1. Symptom Tracking for Chronic and Post-Procedure Patients
You can use voice agents to run short, clinically guided check-ins that capture specific indicators such as:
pain level after a surgery
blood sugar or blood pressure trends reported verbally
Breathing difficulty for respiratory patients
adherence to lifestyle or therapy recommendations
These responses can trigger tasks such as scheduling a review or sending data to your care team.
2. Medication and Treatment Adherence Reminders
For long-term care programs, voice agents can:
Remind patients of scheduled doses
Confirm whether medication was taken
capture reasons for missed doses, which helps clinical teams intervene early
3. Pre-Appointment Preparation and Eligibility Checks
Before a scheduled visit or test, the agent can confirm:
fasting or preparation requirements
availability of insurance documents
presence of prior reports if needed for comparison
whether the patient needs assistance or escort services
This reduces no-shows and ensures smooth patient flow.
4. Post-Discharge Follow-Ups
Instead of relying on manual teams, you can run standardised follow-ups that check for:
new or worsening symptoms
wound care adherence
recovery progress
need for a follow-up consultation
Critical responses can be escalated automatically.
5. Diagnostic Test Workflow Support
Agents can guide patients through steps linked to specific tests by:
confirming sample collection slots
sharing preparation guidelines
capturing rescheduling requests
checking whether reports have been received and understood
6. Patient Experience and Quality Surveys
You can run structured surveys immediately after visits or procedures to measure:
satisfaction with nursing and doctor interactions
wait times
facility experience
discharge clarity
This helps you collect high-quality feedback at scale without additional staff effort.
If your facility handles any of these workflows at scale, automating them helps you maintain consistency, improve preparedness, and give every patient the same level of attention.
Suggested read: AI Voice Assistants in Healthcare: Key Use Cases
Real-World Use Cases from Indian Healthcare Providers
Hospitals and diagnostic networks across India are using voice agents to streamline workflows that need consistency and high-volume execution. These deployments focus on specific operational challenges rather than broad automation goals.
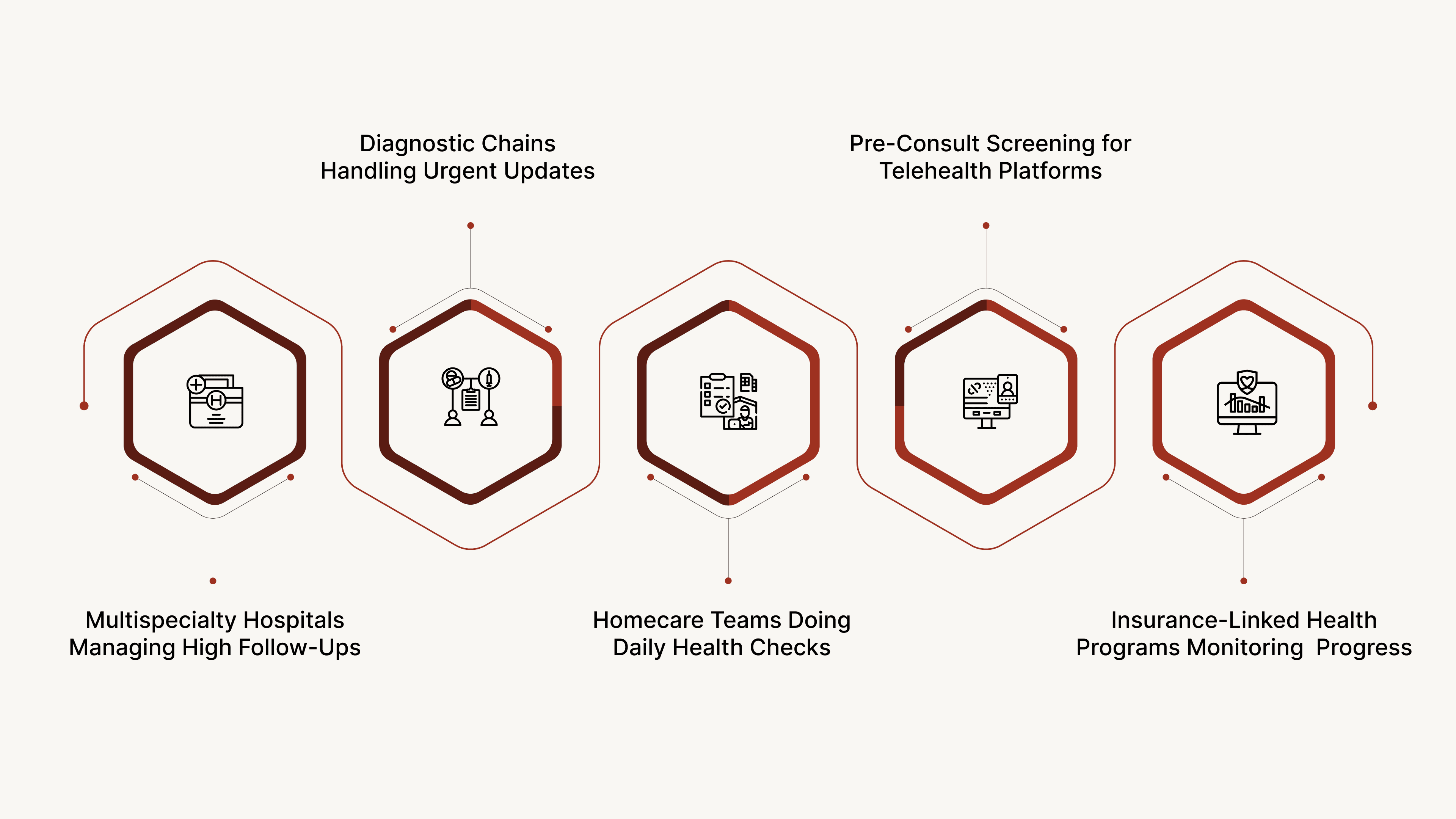
1. Multispecialty Hospitals Managing High Follow-Up Loads
Large hospitals use voice agents to run structured follow-ups for surgical, cardiac, and maternity patients. The agent captures recovery indicators and flags cases that need review. This helps clinical teams focus only on patients who require intervention.
2. Diagnostic Chains Handling Time-Sensitive Communication
Diagnostic networks utilise voice agents to manage preparation instructions and coordinate sample collection. Common tasks include:
sharing guidelines for tests like lipid profiles or ultrasounds
confirming home collection slots
capturing, rescheduling or cancellation requests
checking whether patients received their reports
This reduces inbound call spikes and improves turnaround.
3. Homecare Providers Running Daily Health Checks
Home care services use agents to track the condition of elderly patients or those with long-term conditions. They collect brief, structured updates on mobility, pain levels, appetite, and adherence to therapy. Escalations go directly to the care coordinator.
4. Telehealth Platforms Managing Pre-Consultation Screening
Digital clinics use voice agents to filter basic information before connecting patients to doctors. The agent captures symptoms, verifies condition severity, and routes the case to the right specialty or priority queue.
5. Insurance-Linked Health Programs: Monitoring Patient Progress
Insurance partners coordinating wellness or disease management programs use voice agents to maintain engagement. They track adherence to assigned plans and verify completion of scheduled checkups, which helps in risk assessment and program compliance.
These examples show how voice automation supports different care models. You can adopt similar workflows to reduce delays, improve follow-ups, and give your teams more time to focus on cases that truly need attention.
How to Implement Voice Automation in Healthcare Workflows
Introducing voice automation in a healthcare setting works best when you design it around the way your departments already function. The focus is on aligning automated conversations with clinical protocols, hospital processes, and reporting needs.
1. Select Workflows That Depend on Precise, Repeated Communication
Start with workflows where minor communication lapses create operational issues. Examples include surgeon-led departments that require daily recovery updates, dialysis units that necessitate strict appointment confirmation, or diagnostic departments that rely on accurate preparation instructions for fasting tests. These are areas where automation delivers measurable value immediately.
2. Build Clinical Question Paths With Your Department Leads
For each selected workflow, sit with the respective unit. Orthopaedics may need range-of-movement questions. Cardiology may require breathlessness scoring. Diagnostics may want preparation checks tied to specific panels like LFT or TMT. Creating these paths with department input ensures the agent mirrors the exact protocol your team follows.
3. Define Escalation Criteria Based on Speciality Requirements
Different departments interpret risk differently. A maternity unit may escalate mild cramps, while a general medicine unit may only escalate persistent fever. Set thresholds that reflect your speciality's internal guidelines. This prevents unnecessary alerts and ensures genuine cases are flagged instantly.
4. Decide What Information Must Flow Back Into Your Systems
Hospitals use HIS platforms like Mediware, Napier, Karkinos, or in-house systems. Decide what the agent should write back. For example:
postoperative pain scores into the surgery follow-up sheet
missed medication entries into the chronic care tracker
fasting confirmation in the diagnostics preparation log
Symptom progression into the teleconsultation queue
This ensures that every department is working with the latest data.
5. Pilot With a Department That Has Clear Volumes and Repeatable Patterns
Departments like oncology day-care, dialysis, IVF programs, and radiology often show clean, predictable volumes. A pilot in these units gives you enough data to evaluate automation. Measure outcomes like reduction in no-shows for MRI slots, improvement in recovery tracking for surgeries, or faster triage for teleconsultations.
6. Expand to Multi-Department Deployments Based on Readiness
Once the pilot stabilizes, extend automation to adjacent units. Many hospitals move from surgical follow-ups to maternity, from radiology to pathology, or from chronic care to home care monitoring. This phased expansion keeps changes manageable for your teams.
7. Set Up a Review Loop With Department Coordinators
Each month, review interaction data with coordinators from the participating departments. Look at escalations, patient responses, and missed cases. This review helps you refine question paths, adjust risk criteria, and introduce new workflows that reflect real patient behaviour in your facility.
Once you approach automation step by step, you create a system that fits your protocols and supports your teams instead of disrupting their routine.
CubeRoot Voice AI: Capabilities Tailored for Healthcare Workflows
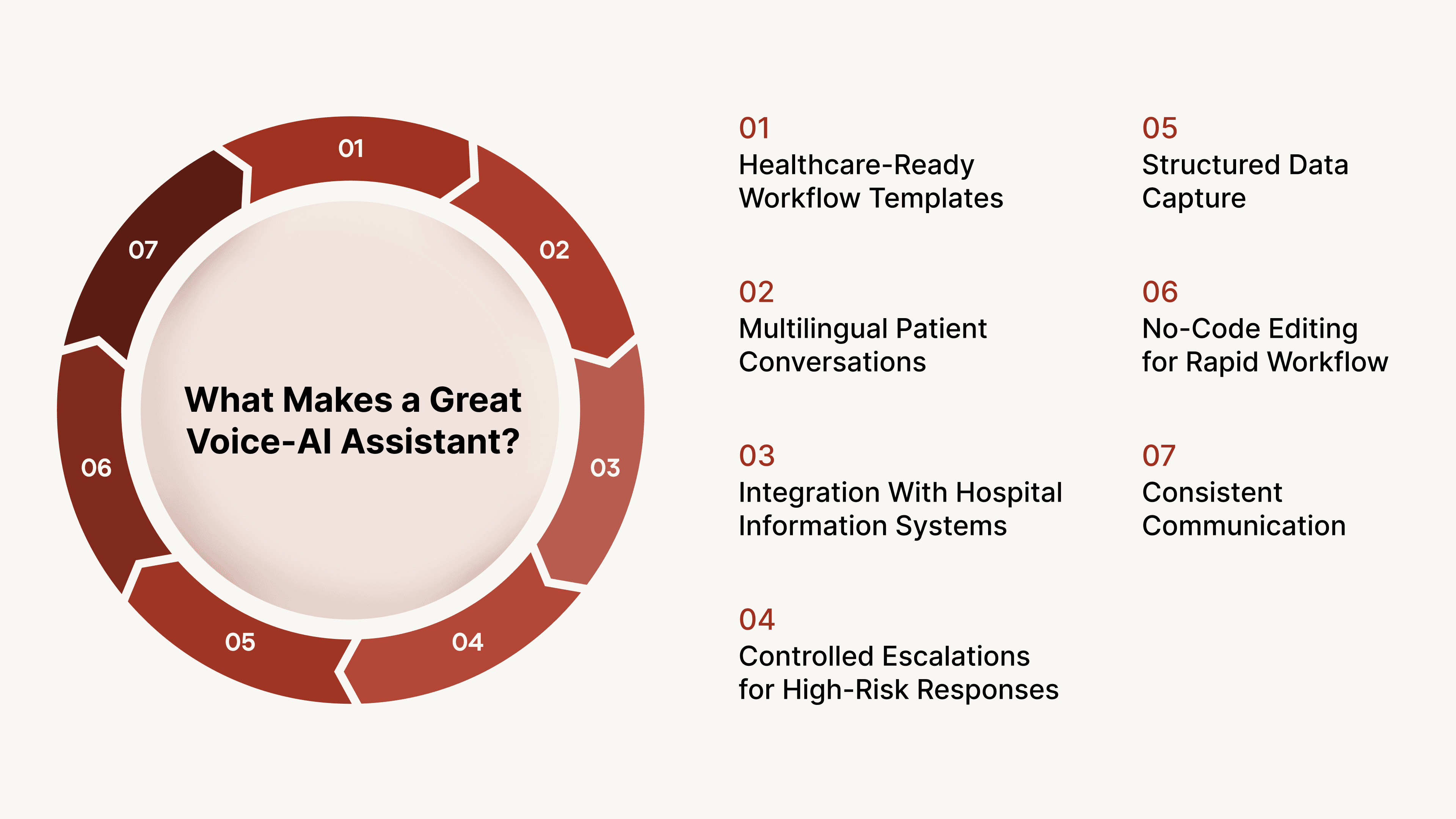
CubeRoot is designed to support communication patterns that Indian hospitals, diagnostic chains, and homecare programs handle every day. The platform focuses on accuracy, multilingual communication, and workflow consistency, which are critical for patient-facing operations.
1. Healthcare-Ready Workflow Templates
CubeRoot provides templates designed with real clinical scenarios in mind. These include postoperative recovery checks, dialysis confirmation flows, maternity follow-up paths, and preparation steps for tests such as TMT, LFT, or ultrasound scans. You can activate these workflows and adjust them to match your department protocols.
2. Multilingual Patient Conversations Across Indian Regions
Patients often respond better when addressed in their preferred language. CubeRoot supports Indian languages such as Hindi, Tamil, Bengali, Marathi, Kannada, and Gujarati. This helps you maintain clarity for patients who may not be comfortable with English or local staff variations.
3. Integration With Hospital Information Systems
CubeRoot connects smoothly with HIS, EHR, and CRM platforms commonly used in India. You can sync appointment data, update follow-up records, send symptom updates to clinicians, and push survey results to your internal dashboards. This keeps every department working with real-time information.
4. Controlled Escalations for High-Risk Responses
Every workflow includes escalation rules that match your internal guidelines. If a cardiac patient reports chest pressure during a follow-up call, the system alerts the coordinator. If a radiology patient is unprepared for a scheduled scan, the slot can be re-evaluated immediately. These controls help you manage risk consistently.
5. Structured Data Capture for Department-Level Insights
CubeRoot records information in a format that is easy to review and analyse. Surgical recovery teams can track pain or mobility trends. Diagnostic departments can see preparation compliance across test types. Homecare teams can identify patterns in daily health checks. This gives your teams evidence that supports operational planning.
6. No-Code Editing for Rapid Workflow Adjustments
Healthcare workflows evolve often. CubeRoot allows your team to update question paths, escalation rules, and department-specific requirements through a simple interface. You can modify a recovery check for a new surgical protocol or adjust a diagnostic preparation flow without relying on developers.
7. Consistent Communication at Any Scale
Whether you need to reach 200 patients from a single department or 50,000 across a diagnostic network, CubeRoot maintains the same clarity and accuracy. This helps you manage communication during periods of high load, such as health camps, corporate screening drives, or seasonal outbreaks.
When you align automation with language needs, specialty workflows, and data requirements, you give your organisation a communication system that stays accurate even as your volumes grow.
Conclusion
Automated voice workflows are becoming a practical necessity in healthcare environments where patient communication needs to be timely, accurate, and consistent. When follow-up checks, preparation guidance, and daily monitoring are handled through structured conversations, departments experience fewer delays and fewer gaps in information.
Hospitals, diagnostic networks, and care programs in India are finding that automated voice interactions help them manage growing volumes without lowering the quality of patient engagement. Clinical teams receive clearer inputs, coordinators spend less time on repetitive calls, and patients get reliable updates without waiting for manual follow-ups. This creates a more stable communication layer that supports the daily rhythm of care delivery.
As more healthcare providers move toward standardised communication processes, voice automation is emerging as a foundational tool for maintaining continuity across departments and ensuring that important patient updates never slip through.
Ready to Modernise Your Patient Communication? Book a quick CubeRoot demo to see how voice automation improves patient communication and reduces operational load.
FAQs
Q: How are AI voice agents different from regular hospital IVR systems?
A: IVR systems follow fixed menu options. AI voice agents understand patient responses, capture structured clinical inputs, and follow department-specific protocols. They can confirm preparation for tests, record symptom progress, and escalate cases that meet defined thresholds.
Q: Can voice agents handle conversations in multiple Indian languages?
A: Yes. Modern voice agents can switch between languages such as Hindi, Tamil, Bengali, Kannada, or Marathi based on patient preference. This is useful for hospitals and diagnostic networks that serve diverse communities.
Q: Do voice agents work for patients who may not be tech-savvy?
A: Yes. Patients only need to answer simple questions on a regular phone call. There are no apps or interfaces to navigate, which makes adoption easier for elderly patients and those managing long-term conditions.
Q: What workflows benefit the most from voice automation in healthcare?
A: Workflows that involve repeated check-ins or time-sensitive instructions see the strongest impact. Examples include surgical recovery checks, dialysis confirmations, test preparation guidance, and monitoring for chronic conditions.
Q: How do hospitals ensure that voice agents escalate the right cases?
A: Escalation rules are set with each speciality. For example, breathlessness in a cardiac follow-up or missed fasting for a test can trigger alerts. These rules ensure that only clinically relevant cases reach coordinators.
Q: Can voice agents integrate with existing hospital systems?
A: Yes. They can read patient details from HIS or EHR systems and update records with new symptom data, preparation confirmations, or survey responses. This keeps all departments aligned with the latest information.























